Help Center
Online Resource Center for Information on Birth Injuries.
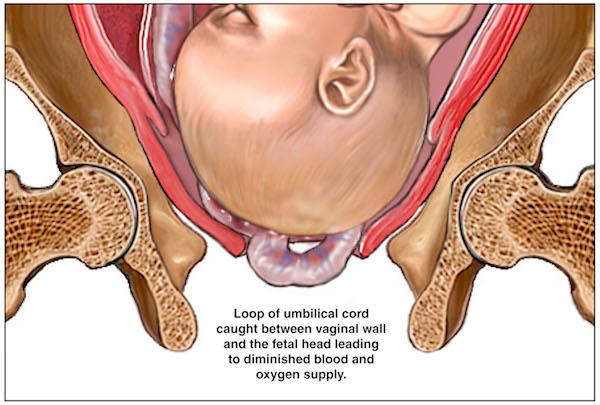
A prolapsed umbilical cord develops when the umbilical cord drops (“prolapses”) through the open cervix into the vagina in advance of the presenting part of the baby. The fear with an umbilical cord prolapse will compress the cord-cutting off the baby’s needed supply of blood and oxygen.
Umbilical cord prolapse is a thankfully infrequent obstetric emergency with an incidence of 0.14 to 0.62% of births. UCP has significant perinatal morbidity and mortality (up to 50% of cases), usually as a result of birth asphyxia from the lack of oxygen to the child.
There is no question that an umbilical cord prolapse is an obstetrical emergency that mandates intervention and immediate delivery of the child.
The umbilical cord is made of two arteries and one vein. The cord moves oxygenated blood from the placenta (attached to the mother) to the fetus. It also removes waste from the fetal bloodstream. The fetus “breathes” (and gets nutrients) from the placenta through the umbilical cord.
In a cord prolapse, the umbilical cord that is normally floating around the baby suddenly descends toward the cervix and the birth canal. This may not cause any problems for the fetus, as long as no pressure is placed on the cord. However, when labor begins, the life-giving cord can become a threat.
In labor, the fetal head moves down against the cervix. Occasionally, the part of the fetus that moves towards the cervix is the buttocks (breech presentation) or a foot (footling presentation). A breech or footling presentation is difficult to deliver vaginally, but when a prolapsed cord is present, it can become much worse.
During the birth process, the head or buttocks can press against the cord without symptoms at first. This pressure may not be obvious to the care provider if the bag of water (amniotic sac) is still intact. The doctor or nurse might only notice a sharp decrease in fetal heart rate. The lowest range of the fetal heart rate is 110 beats per minute, and this will be seen on the labor monitor. If the heart rate dips below this level, or there are significant variable decelerations, these are signs of oxygen deprivation and that Cesarean Section may be needed.
When the mother is already in labor in the hospital, the doctor or midwife can deliberately “break the bag” or rupture the membranes. Often, this is a safe procedure to speed up the process of labor. However, if the fetal head is still too far away from the cervix, the cord can slip over the baby and become part of the flow of amniotic fluid as it leaves the body. The cord can then be seen by the nurse or the doctor. The fetal heart may or may not be affected, but the birth is compromised.
Two major risk factors for cord prolapse complications are polyhydramnios and preterm delivery. In polyhydramnios, too much amniotic fluid is made within the uterus. This increases the chance the cord will fall out when the fluid leaves. In preterm delivery, the small fetus size means the cord can move faster around the baby, and slip out before the birth.
Other risk factors for cord prolapse besides polyhydramnios and prematurity include abnormal fetal presentation (e.g. footling, frank breech), high fetal presenting part, abnormally long umbilical cord, and multiple gestations (twins or more).
When the health care provider has diagnosed a prolapsed cord, three interventions are available. A decision as to which intervention is most appropriate must be done quickly to protect the fetus.
An amnioinfusion is one option. When the mother undergoes an amnioinfusion, a warmed saline solution is delivered into the uterus by a catheter. The purpose of the infusion is to remove the pressure on the umbilical cord by helping the fetus “float” around it. While this is done, the fetal heart rate will be watched constantly.
If the birth is much closer, the doctor must take a different approach. When the baby’s head is already pressed into the birth canal—or if the delivery is happening fast—he or she may ask the mother to get up on her knees and hands to deliver. Obviously, this can only be done if the mother can move. This is not possible if the mother has received a traditional epidural. If the mother needs to change position, the nurse or doula must be available to help her. Once in the hands and knees birthing position, the mother may help the baby to ease off the cord. The baby needs to be born quickly to prevent any further complications.
A Cesarean section will be done if the fetal heart rate is low. If the fetal heart rate does not return to normal, the doctor will place his or her fingers inside the vagina and hold the baby’s head off the cord. This process can be done at any time the prolapsed cord is discovered after the amniotic sac has broken. It can be done by either the doctor or the nurse. Once the care provider has gently pushed the baby’s head off the cord, she will not remove her fingers.
This means that while the mother is transported to the operating room, the nurse or doctor might be on the stretcher with the mother, holding the baby off the umbilical cord. After the baby is removed from the uterus during surgery, the nurse will remove her hand from the vagina.
If the mother feels her “water broke” and suddenly feels the cord coming out with it, she needs to act quickly. First, call 911. Listen to the operator’s instructions. Then call your OB.
You need to listen to medical advice tailored to you. We can tell you the goal is to relieve as much pressure as possible off the baby. You do not want to push. One path that will feel awkward for the mother is getting on her hands and knees with her butt in the air. This can relieve pressure off the cord. (Similarly, during delivery, doctors will often use manual elevation of the fetal presenting part to address compression.)
The mother should resist the temptation to drive to the hospital herself unless instructed to do so. Sitting up or standing will push the baby’s head further into the birth canal.
Also, when the baby’s head moves into place for birth, the mother can feel like she needs to have a bowel movement. She also wants to avoid going to the bathroom! Babies can be born quickly on the toilet by accident.

After the delivery, a pediatrician will examine the baby. He or she will check the Apgar score and may order further lab testing. If the baby not responding, the health care team may perform CPR and administer oxygen. Even if the baby appears normal, she will need to be watched at the hospital. The pediatrician can give the parents more information based on the exam.
Going back to where we started, the fear is oxygen deprivation that can lead to HIE, cerebral palsy, and a host of other birth injuries. If your child suffered any complication where there is a concern about the baby getting oxygen or nutrients from the blood flow to and from the placenta, there may be initial concern. Of course, you need to follow-up with the pediatrician as scheduled. The doctor should address any concerns about the baby’s health or development with the parents if milestones are not being met.
Below are answers and explanations to some of the most frequently asked questions and topics related to umbilical cord prolapse during childbirth.
Umbilical cord prolapse is complication that can occur during childbirth in which the umbilical drops down (prolapses) into the birth canal ahead of the baby. The condition can be very dangerous because when the baby comes down after it will compress the prolapsed cord causes loss of oxygen.
Umbilical cord prolapse is more likely to occur when the baby is in an abnormal presentation (e.g., breech position) or is premature. Too much amniotic fluid (polyhydramnios) is another potential risk factor.
There is no way to prevent prolapse of the umbilical cord from occurring. If diagnosed quickly, however, injury to the baby can be prevent with an emergency C-section. This requires diligent monitoring of mother and baby during labor.
When a prolapsed umbilical cord is being compressed it will cause stress and oxygen deprivation to the baby which can be identified by careful monitoring and analysis of the fetal heart patterns. Certain irregular patterns in fetal heart rates are warning signs of umbilical cord compression.
Fetal hiccups and fetal jerking movements may be a sign of cord compression during pregnancy.