Preeclampsia is a maternal health condition that sometimes occurs in expecting mothers in the later stages of pregnancy. Most women manage preeclampsia quite well. But it creates an increased risk of birth injury, newborn illness, and even fetal and maternal death.
Preeclampsia and related hypertensive disorders during pregnancy cause 500,000 infant fatalities during childbirth annually. So if you have preeclampsia, alarm bells should be going off with your obstetrician to be taking the necessary steps to manage the condition so both you and your child have a safe delivery.
How Common is Preeclampsia?
Still, preeclampsia is not uncommon. Approximately 8% of all pregnant women will be diagnosed with preeclampsia during their pregnancy. Most of these women have mild preeclampsiaPreeclampsia is a progression, as the name suggests, of eclampsia which and refers specifically to convulsions or coma in conjunction with preeclampsia. This can be life-threatening.
When Preeclampsia Occurs
Preeclampsia almost always occurs sometime after week 20 of the pregnancy, with most cases developing during the middle or end of the 3rd trimester. What happens is the preeclampsia causes the blood vessels to constrict. The result is high blood pressure and a reduced blood flow that can affect organs in the mother’s body, including her liver, kidneys, and brain. The mother also faces higher future risk of coronary artery disease.
The diagnosis of preeclampsia is presumed if there is eclampsia, even where signs and symptoms of preeclampsia go undiagnosed before the onset of seizures. Preeclampsia causes concern because it increases the risk of fetal injury and complications for the mother. So it is important that the doctor catches the symptoms and treatment begins promptly.
What Causes Preeclampsia?
The exact physiological causes of preeclampsia are still not fully understood. Research into the underlying cause of preeclampsia is still ongoing but we still only have unproven theories.
The most accepted theory focuses on the placenta and suggests that preeclampsia develops in 2 stages. In the first stage, the placenta produces certain excess proteins that get released into the mother’s system.
The second stage occurs when these excess proteins from the placenta trigger abnormalities in the mother’s blood and cardiovascular system which eventually lead to hypertension and other symptoms of preeclampsia. The excess proteins from the placenta are called antiangiogenic proteins.
Although researchers have a good idea of how and why these antiangiogenic trigger preeclampsia, what is less understood is why the placenta of certain pregnant mothers overproduces these proteins.
The continuing uncertainty about the exact causes of preeclampsia makes it impossible to diagnose preeclampsia in advance. However, there are a number of well-known maternal risk factors which can be used to identify pregnant mothers who are more likely to suffer from preeclampsia than others. The most reliable risk-factors for preeclampsia are maternal obesity prior to and during pregnancy; older mothers (over 35 years); mothers with a prior history of hypertension; and diabetes. Preeclampsia is also more likely to occur if it is the mother’s first pregnancy. Multiples (i.e., twins, triplets, etc.) also make preeclampsia more likely to occur.
We do know is that placental factors are believed to be the cause of preeclampsia. How do we know this? Delivery of the placenta will resolve the maternal symptoms of the disease. So the treatment for pre-eclampsia is delivery of the baby and all products of conception. Until that is done, the preeclampsia will not resolve.
Signs and Symptoms of Preeclampsia
The characteristic symptoms of preeclampsia are maternal hypertension (high blood pressure) and high protein levels in the urine which are triggered by changes in the body during pregnancy.
But these symptoms are harbingers of preeclampsia, not the causes of the syndrome. Preeclampsia is likely caused by from abnormalities in the placenta that feeds the fetus with blood and oxygen. Adequate blood supply is critical for fetal health.
These placental abnormalities often develop in the very early stages of pregnancy, when the vasculature of the placenta is still inchoate. Preeclampsia symptoms also include swelling and rapid weight gain.
The earlier symptoms and indicators of preeclampsia can often be difficult for many pregnant women to recognize themselves because they are often subtle (elevated blood pressure). Other more noticeable symptoms such as swelling can be caused by a number of other things during pregnancy, making it difficult to distinguish between normal body changes during pregnancy and potential red flags. Most cases of preeclampsia are diagnosed by doctors during prenatal care visits.
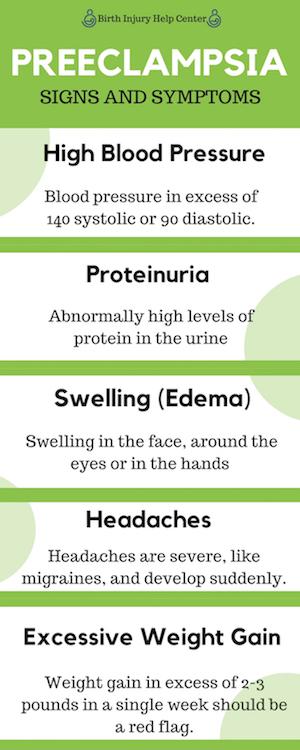
The primary measurable signs and symptoms of preeclampsia are:
- High Blood Pressure: high maternal blood pressure (hypertension) during pregnancy is the most significant indicator that preeclampsia may be developing. For women without a prior history of high blood pressure, hypertension during pregnancy is usually defined as blood pressure in excess of 140 systolic or 90 diastolic. The criteria are different for expecting mothers with higher or lower blood pressure prior to pregnancy. A diagnosis of preeclampsia usually begins with 2 separate high blood pressure readings taken 4 hours apart.
- Proteinuria: abnormally high levels of protein in the urine (proteinuria) is the second key diagnostic indicator of preeclampsia. Normally these proteins remain in the bloodstream or get filtered out by the kidneys and never appear in the urine. However, preeclampsia temporarily disrupts this filtration system. Proteinuria is easily identified by a simple urine test performed in-office during prenatal checkups.
- Swelling (Edema): the most noticeable physical symptom of preeclampsia is often swelling. The problem is that swelling is a normal occurrence that most women experience during pregnancy, particularly in certain areas such as the feet and ankles. This is normal. The type of swelling caused by preeclampsia is known medically as edema and is caused by the buildup of fluid. Swelling in the face, around the eyes or in the hands is not normal and often a sign of underlying issues such as preeclampsia.
- Headaches: headaches are another notable symptom some women with preeclampsia experience. Headaches triggered by preeclampsia are often very severe, like migraines, and develop suddenly.
- Excessive Weight Gain: of course all women naturally gain weight throughout their pregnancy. However, a sudden excess of rapid weight gain can be an indicator of preeclampsia. The reason for this is because preeclampsia causes damage to blood vessels which permits more water to leak into body tissue and stay there instead of being passed through the kidneys and discharged in the urine. Weight gain in excess of 2-3 pounds in a single week should be a red flag.
Managing Preeclampsia
What can you do about preeclampsia? High-quality pre-natal care is critical to effective diagnosis and careful management of preeclampsia. Doctors need to ensure that appropriate consultation by specialists is performed and documented as to potential ongoing signs and symptoms of preeclampsia.
Otherwise, there is a foreseeable probability that ongoing and undertreated preeclampsia will progress to eclampsia and debilitating and/or fatal injury if not resolved. Accordingly, the standard of care is to have a low threshold for treatment and to treat promptly and aggressively, particularly in a patient with symptoms of severe preeclampsia.
Severe Preeclampsia
You do not want to trifle with severe preeclampsia. Marked by the presence of new-onset hypertension and proteinuria, the result can be central nervous system dysfunction (headaches, blurred vision, seizures, coma), marked elevations of blood pressure, severe proteinuria, oliguria or renal failure, pulmonary edema, hepatocellular injury, thrombocytopenia, or disseminated intravascular coagulation. Particularly severe cases of preeclampsia can cause more serious issues such as low platelet levels, breakdown of red blood cells, or impaired kidney and liver functioning.
Recent Medical Literature on Preeclampsia
Preeclampsia is being studied rigorously due to its status as one of the top health issues that affect mothers and babies. The biological mechanisms that underlie preeclampsia and the best tests to identify who is at risk for preeclampsia and related complications are some of the topics researchers are interested in clarifying. Some of these recent studies are listed below.
- “Screening and Prevention of Preeclampsia” by Liona C. Poon, et al., Maternal-Fetal Medicine, 2019.
Preeclampsia (PE) is a pregnancy disorder characterized by hypertension that is one of the leading causes of maternal and prenatal illness and mortality. Traditional methods of screening, as recommended by professional guidelines, have limited doctors’ ability to predict if a patient will develop preeclampsia. According to this study, doctors should better screen for pre-term preeclampsia (w/less than 37 weeks’ gestation). Additionally, they find that the best way to identify high-risk groups is the Bayes-based method. The Bayes theorem in statistics is used to determine the probability of an event based on past conditions, so the researchers in this article suggest combining a patient’s medical and obstetric history with numerous test results. - “Aspirin versus Placebo in Pregnancies at High Risk for Preterm Preeclampsia” by Daniel L. Rolnik, M.D., et al., the New England Journal of Medicine, 2017.
The aim of this study was to determine whether the intake of low-dose aspirin during pregnancy can reduce the risk of preterm preeclampsia. 1,776 pregnant women at high-risk for preeclampsia were randomly assigned either a low dose of aspirin or a placebo from 11-14 weeks of gestation until 36 weeks gestation. The results showed that treatment with low-dose aspirin in women at high risk for preterm preeclampsia showed a lower incidence of diagnosis than placebo. This study supports the recommendation of the American College of Obstetrics and Gynecologists that women at risk for preeclampsia take low-dose aspirin from 12-24 weeks gestation until delivery. - “Preeclampsia: Updates in Pathogenesis Definitions, and Guidelines” by Elizabeth Phipps, et al., Clinical Journal of American Society of Nephrology, 2016.
This article is an overview of the causes, outcomes, and recommendations for preeclampsia. Preeclampsia has become an increasingly common diagnosis in the developed world and is still a leading cause of maternal and fetal morbidity and mortality in the modern world. Risk factors of the condition include maternal age, obesity, and vascular diseases, to name a few. In this review the most recent research on the “pathogenesis,” or origin, of preeclampsia is discussed. One of the reasons that preeclampsia is so prevalent is inadequate prenatal care. However, the researchers are optimistic about the future care of women with the condition as scientific understanding continues to improve. - “Evaluation of the clinical impact of the revised ISSHP and ACOG definitions on preeclampsia” by Anisha R. Bouter and Johannes J. Duvekot, Pregnancy Hypertension, 2019.
In 2013 and 2018, both the Society for the Study of Hypertension in Pregnancy (ISSHP) and the American College of Obstetricians and Gynecologists (ACOG) revised their criteria for the diagnosis of hypertensive disorders in pregnancy. The diagnosis of preeclampsia previously relied on the presence of hypertension and proteinuria (excess protein in urine), however the 2013 revision stated that the diagnosis of preeclampsia can be established without the presence of proteinuria when other specific symptoms are present. In 2018, the second change was made due to the recognition of maternal and fetal risk in non-proteinuric preeclampsia. More cases of the condition were found when non-proteinuric preeclampsia cases were included. The objective of this study was to look at the clinical impact of the three new definitions in the diagnosis of preeclampsia. The authors conclude that more research is needed about non-proteinuric preeclampsia. - “Pregnancy-Related Acute Kidney Injury in Preeclampsia: Risk Factors and Renal Outcomes” by Frances I. Conti-Ramsden, et al., Hypertension, 2019.
Preeclampsia is a common cause of acute kidney injury (AKI), however its risk factors and consequences for the kidneys are unknown. This study of 1,547 women admitted to the hospital with preeclampsia looks at baseline demographics, admission characteristics, and maternal and neonatal outcomes. Women who developed an AKI were more likely to die, have an eclamptic seizure, have a stroke, have received magnesium sulfate, and be admitted to intensive care compared with women who did not develop an AKI during admission with preeclampsia. The most important finding was that maternal death, eclampsia, stroke, and stillbirth rates were significantly higher in women admitted with an AKI than in those without. This data suggests that AKI may be a useful marker of maternal disease severity in preeclampsia, warning doctors when there is a high risk of danger so that they can be ready to treat the worst. - “Placental growth factor predicts time to delivery in women with signs or symptoms of early preterm preeclampsia: a prospective multicenter study” by John R. Barton MD, MS et al., American Journal of Obstetrics and Gynecology, March 2020
This study, published just last month, looked at “placental growth factor” as a predictor of when a woman with signs of preterm preeclampsia will deliver her child. It is extremely useful for doctors to know if and when a woman will go into labor prematurely. Placental growth factor (PGF) is a protein that plays an important role in the vascular formation of a human embryo. Doctors can measure this protein in pregnant women. The study examined 753 women with signs of preeclampsia enrolled at 24 health centers. A low PGF in women with suspected preeclampsia at less than 35 weeks’ gestation was correlated with preterm delivery. The study finds that PGF may be a better predictive tool for doctors than clinical markers that are currently used. - Wintertime Wood Smoke, Traffic Particle Pollution, and Preeclampsia by Vanessa Assibey-Mensah et al., Hypertension, January 2020.
Researchers are still working to understand the mechanisms in the body behind preeclampsia and what triggers the condition. This study draws on previous studies that suggested a link between air pollution and preeclampsia. Using data from Monroe County, New York, researchers found that each 3.64 µg/m3 increase in pollution levels—in this case woodfire and traffic pollution—increased the odds of early-onset preeclampsia. They did not find a link, however, to late-onset preeclampsia.