Postpartum endometritis is an infection of the uterus lining or upper genital tract that some women develop following childbirth. The term “postpartum” refers to the period of the time right after childbirth and “endometritis” is a reference to the location of the infection in the endometrium. The endometrium is the interior wall of the uterus. This inner uterine wall is where the post-delivery bacterial infection occurs with this condition.
Is postpartum endometritis life-threatening? No, this infection is life-threatening in the rarest of cases. But it can cause a fever, stomach pain, vaginal bleeding… all things you do not want to be dealing with under any circumstances, much less while caring for a newborn. So you want to understand this infection and treat it as effectively as possible.
What Causes Postpartum Endometritis?Postpartum endometritis is a bacterial infection, so it is caused by the infiltration of bacteria into the inner lining of the womb.
The bacteria typically migrates into the endometrium during the labor and delivery process and grows into a full-blown infection in the following days or weeks.
Postpartum endometritis infections usually develop fairly soon after delivery. Most cases are diagnosed within the first 10 days after childbirth. However, postpartum endometritis can sometimes take longer to develop and the condition can occur anytime within the first 6 weeks after delivery.
Endometritis postpartum can be caused by any type of bacterial, but the most common pathogens involved in this infection are group B streptococci and staphylococcus (staph).
Risk Factors for Postpartum Endometritis
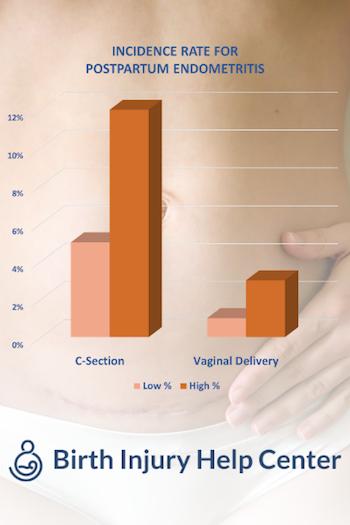
Postpartum endometritis is much more common post-C-section delivery compared to a normal vaginal delivery. After a regular, vaginal delivery, the reported incidence rate of postpartum endometritis is about 1-3%. The incidence rate for postpartum endometritis is 5-10 times higher after a C-section delivery. This makes a C-section delivery the primary risk factor for this condition.
Aside from C-section delivery, other known risk factors that make postpartum endometritis more likely to develop include:
- Prolonged labor: postpartum endometriosis after birth is more common after prolonged labor where a long period passes between the rupture of the fetal membranes and delivery, internal infections are more likely to occur.
- Maternal Infection: if the mother develops an infection during pregnancy (or has an active infection when she goes into labor) she is more likely to develop postpartum endometritis.
- Internal Examinations: if doctors or nurses perform a lot of internal examinations during labor and delivery it will increase the risk of bacteria getting into the womb and developing into postpartum endometritis.
What Are the Symptoms of Postpartum Endometritis?The primary symptom associated with postpartum endometritis is fever. An elevated temperature is almost always one of the first symptoms of this condition and it occurs in just about every case. Other common symptoms include:
- Pain or mild swelling in the abdomen
- Abnormal smelling vaginal discharge
- Pain during sex or urination
The problem with identifying the symptoms of postpartum endometritis is that it can be difficult to tell what is normal in the weeks after giving birth.
How Does Placental Removal Tie into Endometritis?Doctors remove the placenta in one of two ways. The first is to wait for the placenta to separate from the uterus. The second is the doctor can take her hand and form a cleavage plane between the placenta and the wall of the uterus. The latter is called manual removal of the placenta. This increases the likelihood of postpartum endometritis. Why? Because you are breaking up blood vessels. This causes more raw surfaces to emerge which are breeding grounds for preexisting bacteria in the endometrial cavity.
What Are Postpartum Endometritis Symptoms?
- Fever (main symptom, usually with 3 days of childbirth
- Uterine tenderness
- Vaginal bleeding in between your normal menstrual cycle
- Smelly vaginal discharge
- Pain during urination
- Stomach pain or swelling
Postpartum endometritis is initially diagnosed through physical examination and observation of endometritis postpartum symptoms. This may include a vaginal examination or swab. The diagnosis can be confirmed through blood and urine testing.
If you have these symptoms post-C-section, doctors will highly suspect postpartum endometritis.
Diagnosis and Treatment of Postpartum Endometritis
Most cases of postpartum endometritis can be effectively treated with basic antibiotics that you take at home. The 2nd generation antibiotic clindamycin is usually prescribed in combination with another type of antibiotic (usually gentamicin). These are often given by injection in an outpatient setting. In some cases, women with postpartum endometritis may be treated in a hospital setting and given antibiotics intravenously.
What Are the Risks and Complications of Postpartum Endometritis?As long as postpartum endometritis is diagnosed quickly, it can usually be effectively treated without any long-term health implications. When the condition is not immediately diagnosed, however, it can spread very quickly inside the women’s body. If endometritis postpartum goes undiagnosed and untreated, the worst-case scenario is that it could progress into sepsis. Sepsis is an infection in the bloodstream that can often be fatal.
Are Prophylactic Antibiotics Wise to Prevent Postpartum Endometritis?Prophylactic antibiotics are an option to prevent postpartum endometritis, especially for women who have a C-section. Vaginal cleaning before delivery has also been shown to reduce the risk of postpartum endometritis?
Medical Literature on Postpartum Endometritis
We link to a good bit of medical literature on postpartum endometritis above. Here are some more articles if you are looking to take a deeper dive into the topic.
- Baksu A, et al: The effect of placental removal method and site of uterine repair on postcesarean endometritis and operative blood loss. Acta Obstet Gynecol Scand 2005; 84:266.
- This study looked at whether C-section-related blood loss and postpartum endometritis were associated with placental removal methods and uterine repair sites. The researchers found that a manual placenta removal during a C-section yielded significant blood loss and higher postpartum endometritis rates.
- Chaim W, et al: Prevalence and clinical significance of postpartum endometritis and wound infection. Infect Dis Obstet Gynecol 2000; 8:77.
- This study looked at potential clinical variables associated with postpartum endometritis and wound infections. The researchers found that premature birth, severe pregnancy-induced hypertension, fetal distress, postpartum anemia, neonatal mortality, and Apgar scores lower than seven were associated with postpartum endometritis. They also found that gestational diabetes, previous C-sections, and low Apgar scores were associated with wound infections.
- Chainarong, N., Deevongkij, K., & Petpichetchian, C.: Secondary postpartum hemorrhage: Incidence, etiologies, and clinical courses in the setting of a high cesarean delivery rate. PloS one 2022; 17: e0264583.
- This study looked at secondary postpartum hemorrhaging’s incidence, etiologies, and clinical outcomes in a hospital with a high C-section rate. The researchers examined 123 women who were hospitalized for secondary postpartum hemorrhaging. The researchers found that 52 percent of these women underwent a C-section. They also found that over 67 percent of cases involved postpartum endometritis, over 80 percent of which involved C-sections. However, the C-section group also experienced lower retained placental tissue rates. The researchers concluded that women who underwent C-sections were at high risk for postpartum endometritis, but at low risk for retained placental tissue.
- Eslamian, L., & Nouri, B.: Severe Parametritis after Vaginal Delivery with Delayed Response to Broad Spectrum Antibiotics: A Case Report. Novelty in Biomedicine. 2021; 9: 149-151.
- This case study examined a patient who experienced severe parametritis within 24 hours of a delivery. The researchers that the patient suffered a severe pelvic infection following a vaginal delivery. They also found that a prolonged membrane rupture was the infection’s risk factor. The researchers concluded that a timely diagnosis and treatment would help prevent abscess and sepsis.
- Hamdy, M. A., Taha, O. T., & Elprince, M.: (2021). Postpartum endometritis after uterine cleaning versus no cleaning in cesarean sections: Randomized clinical trial. Journal of Obstetrics and Gynaecology Research 2021; 47: 1330-1336.
- This study looked at the association between postpartum endometritis and uterine cleanings that followed an elective C-section. The researchers recruited expectant mothers who chose to undergo a C-section. They allocated them into two groups. One underwent a uterine cleaning, while the other did not. The researchers found that the postpartum endometritis rate was 3.6 percent in the cleaning group and 0.3 percent in the control. They also found that the blood loss and septic wound infection rates were higher in the cleaning group. The researchers concluded that uterine cleanings were associated with increased blood loss and postpartum endometritis rates. They also concluded that surgical teams can omit uterine cleanings.
- Hidar, S., et al: The effect of manual removal of the placenta on post-cesarean endometritis. Obstet Gynecol 1996; 87:99.
- This study looked at whether placental removal methods that followed a C-section impacted perioperative hemorrhaging and maternal infectious morbidity. The researchers found that routine manual placenta removals increased postpartum infection and perioperative blood loss risks.
- Knight M, et al: Prophylactic antibiotics in the prevention of infection after operative vaginal delivery (ANODE): a multicentre randomised controlled trial. Lancet 2020; 393:2395.
- This report looked at the risks of taking prophylactic antibiotics for the prevention of maternal infections that follow vaginal deliveries. The researchers concluded that maternal infection prevention requires general measures to prevent infection in all women during and after birth. They also concluded that healthcare providers must consider the effectiveness of prophylactic antibiotic use in different settings.
- Puente E, et. al: Chronic endometritis: old problem, novel insights, and future challenges. Int J Fertil Steril 2020; 13: 250-256.
- This review looked at the current literature involving chronic endometritis and synthesized findings that were retrieved from computerized database searches. The researchers found that effective antibiotic treatments improved the live birth and pregnancy rates in patients suffering from repeated miscarriages and increased the ongoing pregnancy rate in patients suffering from recurrent implantation failure.
- Salem, M. A. A., Soliman, A. Z. M., & Ammar, I. M. M.: Effect of clindamycin vaginal pessary before cesarean section on postpartum infectious morbidity. Microbes and Infectious Diseases, 2022.
- This study looked at the association between clindamycin administration before an elective C-section and postpartum infections. The researchers included 196 patients. Half of them received clindamycin, while the other half received nothing. The researchers found that the clindamycin group experienced lower fever, wound infection, endometritis, and post-C-section infection morbidity rates than the control group. They also found statistically significant differences in white blood cell and C-reaction protein level rates. The researchers concluded that administering clindamycin before an elective C-section reduced the postpartum infection, fever, wound infection, and post-C-section infection morbidity rates